Thursday, May 31, 2012
Effects of Load-Bearing in Cerebral Palsy: Bones
The intent of this post is two-fold: 1) to discuss and explore a very relevant, critical, yet controversial subject of dicussion within Cerebral Palsy (CP) (and other disorders of movement and posture)...2) to link previous posts together with this one to shape a formulate the overall narrative. As always, my overall intention is not to discredit any particular school of thought, strategy, or central philosophy...rather to bring the realities of the mechanical challenegs (and consequences) that accompany CP to the forefront so that specific, goal-oriented strategies can be formulated. It should be clear that these strategies are case specific and therefore need to be evaluated with it´s own set of standards.
This first installment will focus on the direct effect of load-bearing (weight-bearing) on the bones. However, before any in-depth discussion begins, I should define what load-bearing means within the context of this post. To be very specific, load bearing is: exposing an architectural system to structural load or stress. Therefore, in the human organism this is very clearly achived in either a seated or standing position.
The benefits of load bearing or weight bearing in the healthy person are quite obvious and straightforward...the ground force reaction promotes to development of growing bones and contributes to the development of healthy bone density. Although this is very true, the fundamental mistake that is quite often made is that this statement is imported to the CP community. Why is this a mistake? This statement assumes that the transmission of ground force reaction is efficient and therefore travels to the relevant load bearing structures throughout the body...in disorders of movement and posture (CP, for example), force transmission is extremely disrupted and inefficient. This disruption leads to improper stress distribution, accessory and compensatory activation of skeletal muscle, overuse and fatigue syndromes, as well as structural deterioration. To be very clear: mechanical forces in the CP individual DO NOT travel in a manner that facilitates healthy growth and development.
I doubt any responsible professional would debate this fact...however, a fundamental question is therefore raised: if this is an understandable fact, why is there such a rush to implement "standing" protocols? This is a glaring contradiction that generally goes unseen, but certainly exists...and therefore needs to be addressed.
In order to address this delicate topic intelligently and responsibly, we need to dissect the effects of load bearing into some fundamental component parts: the effect on the bony skeleton itself and the effect on the soft tissue. The effects on the system as a whole are actually greater than the sum of the component parts, but far more complex...therefore a basic understanding of the component parts should give some clarity on the potential "biomechanical tax" that is paid when weight bearing is aggressively promoted.
MECHANOTRANSDUCTION IN BONES: If the term Mechanotransduction is new to you, i would refer you to my previous post titled "Mechanotransduction: Response to Manual Therapy". However, to summarize the concept, it is the cellular response to mechanical forces or loads. The precise mechanism in which bones sense mechanical stimulii is still largely being researched, however the concept of cellular mechanotransduction in the bones is widely accepted as a likely mechanism. With respect to the skeleton, there is an integration of the understanding of the connective tissue memebrane of the bone (periosteum), cellular tensegrity, and the effects of mechanotransduction on the nucleus of the osteoblast. Effectively, mechanical stress and deformation that is load-induced activates a change in the genetic program of the bone (gene transcription). Mechanical information is relayed from the bone to the gene by a succession of long-term deformation and changes in conformation. If the stresses applied to the bone are not distributed properly, skeletal growth and absorption are disrupted...which leads to eventual bony deformation and therefore impaired function.
Although this is a common understanding in the field of cellular biochemistry, it doesnt seem to reach the professional "masses" to be applied responsibly in rehabilitative protocols. Given this knowledge, it becomes clear that consistent, intensive, and aggressive strategies geared towards standing protocols (standers, for example) is potentially costly when you consider the "biomechanical tax" to be paid in the long-term. Although bony misalignment is a reality in the CP individual, load bearing and exposing an altered structural "scaffold" to loads exacerbates the deterioration of structural integrity.
Although significant, this is only part of the overall perspective. The effects of load bearing with respect to the soft-tissue will be the subject of the second load-bearing post. Hopefully both or either will stimulate some analytical thought on the subject and consequenty result in more informed and effective strategies.
Cheers.
Wednesday, May 23, 2012
The Activ8 System
After a few trials, many format changes, and quite a bit of hesitation...I have finally decided to present my long-overdue fitness protocol for professionals. I had originally presented it a year ago as Soft Plyometrics, however I have refined it in an effort to make it as compact and useful as possible. More importantly, something that can be implemented very easily and very quickly. The Activ8 System is a tool designed to tap the body´s undiscovered performance potential. It includes very specific strategies and guidelines, however it is fundamentally a philosophy. The philosophy is based in the idea that performance potential (and even general health) is multi-rooted and multi-faceted...therefore it simply cannot be fully cultivated unless each root and each facet are stimulated. The beauty of the Activ8 System is that it doesn´t ignore or disregard ANY other fitness paradigm...in fact, it absorbs it. It can be implemented as a complete health, wellness, or fitness platform...or it can be inserted as a compliment to any and all fitness protocol. The adaptability of Activ8 is due to the fact that it´s primary objective is the development of the most primitive and fundamental structures involved in human deveopment and performance: Connective Tissue. Beyond the obvious strategic objectives of increased strength, power, endurance...the connective tissue / fascial system is responsible for important elemental and integral functions such as fluid transport, metabolic homeostasis, and the regulation of the injury repair mechanism.
The full protocol will be unveiled here over time, however I will be attempting to initiate some trial runs with a couple of enlightened professionals (check out Fitnophrenia blog at getcrazyfit.blogspot.com as well as my good friend Simon at Balance Fitness on Facebook) ahead of time to get the ball rolling. Until then, the fundamentals of the Activ8 System should be outlined. As you may have guessed, there are 8 central objectives:
Strengthen. Develop and increase overall strength by promoting one of the fundamental elements in force transfer and distribution---Fascia. Relax. Implement effective and efficient active relaxation strategies to reduce muscular stress and fatigue. Nourish. Actively promote and assist the flow of nutrients throughout the body to increase regeneration and repair. Repair. Implementation of strategies to combat overuse syndromes, chronic and acute injury, inflammation, and the buildup of metabolic by-product. Facilitate. Facilitate and improve the positive effects of complimentary protocols and interventions. Support. Actively develop the primitive support structures that are used, not only in performance situations, but in daily life as well. Maintain. The maintenance of general health and metabolic homeostasis. Develop. Develop the fundamental building blocks for long term health and fitness.
More to come!
Tuesday, May 22, 2012
Stretching and Cerebral Palsy: What you should know.
This is something I would most certainly define as a ¨hot button topic¨. Although most would consider it a relatively straightforward issue, the reality is that there are many schools of thought on this particular issue...all of which typically claim to have the ¨correct¨ perspective on the subject. It has been my experience that most take an all-or-nothing approach...black or white...do or don´t...stretching in Cerebral Palsy (CP) is good / stretching in CP is bad. I certainly have a specific position in the matter, however I think it is more productive to for people (both professional and health care seeker) to arrive to their own conclusions and convictions. This relatively trivial and non-sensical debate becomes completely irrelevant once the reality of the CP condition is analyzed in any decent way. I don´t think that there is any requirement to go into detail about the implied rationale for stretching...this is something that, to say the least, is well understood. However, a broad look into ¨what is stretching¨ will help to frame the overall message of this post.
Stretching is most commonly performed to achieve a specific end result: elongation of a particular muscle or group of muscles. This seems relatively intuitive and would make sense to any lay person. The part that is not so intuitive is that the muscles themselves are embedded within a connective tissue matrix...which is in turn blended with other differentiated connective tissue (tendon) that is continuous with the outer layer (periosteum) of the bone. From there, the periosteum continues and eventually blends once again and the kinematic chain continues.
Therefore it becomes quite clear that it is next to impossible to selectively isolate muscle tissue from the connective tissue matrix / system it exists with..in fact, they are inseperable and synonymous with each other. In other words, ¨stretching the muscle¨ effectively results in applying tensional force throughout the entire system (muscle, epimysium, perimysium, fascia, tendon, ligament, periosteum, etc...). In order to further decontruct the entire stretching concept, the terms muscle and connective tissue need to be further defined.
Muscle is defined as a tissue composed of bundles of elongated cells capable of contraction and relaxation to produce movement. Connective Tissue can be descried as a tissue developed from the embryonic mesoderm that consists of collagen or elastic fibres, fibroblasts, fatty cells, etc., within a jelly-like extracellular matrix. It supports organs, fills the spaces between them, and forms tendons and ligaments. Knowing these basic facts and definitions, their respective functional appearances within the normal muscle and the spastic muscle (CP) need to be defined. They should be the same, right? This couldnt be further from the truth. This is what the current (and most popular)approach assumes...that muscle is muscle and fascia is fascia. I have attached a very interesting and informative study that was performed to identify the similarities / differences between spastic and normal muscle tissue, spastic and normal extracellular matrix, as well as the differences between individual cells and collective bundles of cells for both. I recommend that you take the time to read it, but I will summarize its contents here in an effort to expediate my point (it´s effectively the abstract of the article): 1) The difference between bundles and single cells was much greater in normal muscle tissue (16 times stronger) than in spastic muscle (2 times stronger). 2) Actual muscle fiber strength is greater in spastic muscle than in normal muscle. However..... 3) Extracellular matrix strength / Connective Tissue strength is 43.5 times weaker!! Therefore, the ¨inconvenient truth¨ is exposed and a fundamental question is raised: if the spastic muscle itself is stronger than normal muscle, and the connective tissue attachments are 43 times WEAKER...what is really happening when you attempt to stretch that particular muscle(s)? In my professional opinion, it seems only logical that the likely result is further weakening and de-stabilization of an already weak connective tissue system...however, I am more than willing to set that staunch opinion aside if ever there was a way to guarantee this wouldn´t happen. The current reality is that, at best, there is no definite way to determine if the attempts to relax spastic muscles via stretching will not potentially be of some detriment. Indeed, there are some cases where some relief has been attributed to active stretching...however, these responses are transient and were most likely done in a very mild form.
The article goes into more important details (muscle fiber size and area is smaller in spastic muscle, for example), so I will leave those for the more curious to digest. In summary, I do not belong to the extreme end of the continuum in saying that ¨all stretching is bad¨ and that it absolutely shouldnt be done. My main message is that proper consideration be made to the actual mechanical and physiological benefits / consequences of ANY therapeutic intervention. If, through careful thought, consideration, and analysis, stretching is indicated...then it is obviously worthy of implementation. The harsh reality is that many forms of stretching are dispensed without any constructive analysis...which is fundamentally dangerous. To put a final point on this topic...forget about absolute ¨black and white¨solutions. There is a whole lot of grey to choose from! Cheers! Inferior Mechanical Properties of Spastic Muscles Due to Compromised Extra Cellular Matrix Material
Stretching is most commonly performed to achieve a specific end result: elongation of a particular muscle or group of muscles. This seems relatively intuitive and would make sense to any lay person. The part that is not so intuitive is that the muscles themselves are embedded within a connective tissue matrix...which is in turn blended with other differentiated connective tissue (tendon) that is continuous with the outer layer (periosteum) of the bone. From there, the periosteum continues and eventually blends once again and the kinematic chain continues.
Therefore it becomes quite clear that it is next to impossible to selectively isolate muscle tissue from the connective tissue matrix / system it exists with..in fact, they are inseperable and synonymous with each other. In other words, ¨stretching the muscle¨ effectively results in applying tensional force throughout the entire system (muscle, epimysium, perimysium, fascia, tendon, ligament, periosteum, etc...). In order to further decontruct the entire stretching concept, the terms muscle and connective tissue need to be further defined.
Muscle is defined as a tissue composed of bundles of elongated cells capable of contraction and relaxation to produce movement. Connective Tissue can be descried as a tissue developed from the embryonic mesoderm that consists of collagen or elastic fibres, fibroblasts, fatty cells, etc., within a jelly-like extracellular matrix. It supports organs, fills the spaces between them, and forms tendons and ligaments. Knowing these basic facts and definitions, their respective functional appearances within the normal muscle and the spastic muscle (CP) need to be defined. They should be the same, right? This couldnt be further from the truth. This is what the current (and most popular)approach assumes...that muscle is muscle and fascia is fascia. I have attached a very interesting and informative study that was performed to identify the similarities / differences between spastic and normal muscle tissue, spastic and normal extracellular matrix, as well as the differences between individual cells and collective bundles of cells for both. I recommend that you take the time to read it, but I will summarize its contents here in an effort to expediate my point (it´s effectively the abstract of the article): 1) The difference between bundles and single cells was much greater in normal muscle tissue (16 times stronger) than in spastic muscle (2 times stronger). 2) Actual muscle fiber strength is greater in spastic muscle than in normal muscle. However..... 3) Extracellular matrix strength / Connective Tissue strength is 43.5 times weaker!! Therefore, the ¨inconvenient truth¨ is exposed and a fundamental question is raised: if the spastic muscle itself is stronger than normal muscle, and the connective tissue attachments are 43 times WEAKER...what is really happening when you attempt to stretch that particular muscle(s)? In my professional opinion, it seems only logical that the likely result is further weakening and de-stabilization of an already weak connective tissue system...however, I am more than willing to set that staunch opinion aside if ever there was a way to guarantee this wouldn´t happen. The current reality is that, at best, there is no definite way to determine if the attempts to relax spastic muscles via stretching will not potentially be of some detriment. Indeed, there are some cases where some relief has been attributed to active stretching...however, these responses are transient and were most likely done in a very mild form.
The article goes into more important details (muscle fiber size and area is smaller in spastic muscle, for example), so I will leave those for the more curious to digest. In summary, I do not belong to the extreme end of the continuum in saying that ¨all stretching is bad¨ and that it absolutely shouldnt be done. My main message is that proper consideration be made to the actual mechanical and physiological benefits / consequences of ANY therapeutic intervention. If, through careful thought, consideration, and analysis, stretching is indicated...then it is obviously worthy of implementation. The harsh reality is that many forms of stretching are dispensed without any constructive analysis...which is fundamentally dangerous. To put a final point on this topic...forget about absolute ¨black and white¨solutions. There is a whole lot of grey to choose from! Cheers! Inferior Mechanical Properties of Spastic Muscles Due to Compromised Extra Cellular Matrix Material
Wednesday, May 16, 2012
Life, Tensegrity, and Thermodynamics
The title of this post is likely to deter most casual readers and appeal to the few ¨nerds¨ out there...so I expect a relatively low number of reads. However, I hope it inspires some analytical thought and stimulates some curiosity. At the very least...it´s interesting!
I have to give credit to Mr. Serge Gracovetsky who is a well known researcher (from my home town of Montreal, no less) who has been well ahead of the curve with respect to ¨how the body really works¨. His enormous body of work is something to behold and should be an essential component to any serious clinician´s resource library. His insights and concepts are the essense behind this post...I simply ¨dumb them down¨ for my own consumption.
Although the terms Tensegrity and Thermodynamics are quite straightforward, ¨LIFE¨ is a term that is obviously something subject to interpretation...and therefore it is unlikely that a true ¨definition¨ will ever be found. However, in the functional sense, life is the convertion of heat into energy. Living organisms are essentially converters that transform heat into mechanical work. This convertion (heat into mechanical work) is extremely inefficient however...the classic steam engine was only 3% efficient!! This is due to the Second Law of Thermodynamics: Energy continuosly degrades and is less and less available for work. This energy loss is called ENTROPY. Since energy is continuosly lost, entropy increases over time.
In order for life to exist (and persist), this energy loss and entropy has to be minimized...therefore ¨life¨ exists in the most energy efficient and low energy cost state (for example, water, salts and minerals crystallize) that is also stable. Therefore...as Gracovetsky states...To survive the animal must minimize its energy needs, that is minimize the rate at which the entropy increases.
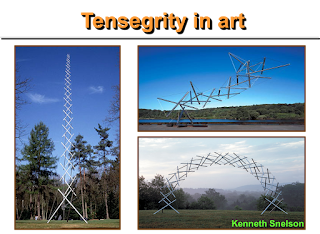
What does this all mean? Organisms driven purely by muscle would be efficient in a fluid medium (like fish, for example...essentially all muscle and very little solid bone and connective tissue), however in a gravitational field (on the earth) muscles are extremely expensive energy users. Therefore, LIFE has blessed us with Tensegrity...which essentially allows us to be upright in a gravitational field without using muscles all the time. Tensegrity is a technique for building structures by decomposing forces into their compressive and tensile components.
The marvel of tensegral structures is that they are highly adaptable to stress and can therefore support loads without experiencing structural failure. Within the human organism, one of the most prevalent tensile structures is Collagen.
In summary, this simple realization should signal a radical shift in current ¨standards¨ of practice in traditional rehabilitative sciences. It essentially presents a challenge to the conventional, classicla representation and modelling of biomechanical systems (Gracovetsky).
Mr. Gracovetsky could not have summarized this very important point more clearly: The response of tissues under stress should not be limited to the mechanical properties of the tissues, but should include the dynamic reconfiguration of the collagen network. Such a desirable analysis is unfortunately not the norm in the literature.
...Hopefully a good read for nerds and non-nerds alike!
Cheers!
Tuesday, May 8, 2012
Connective Tissue: Extracellular Matrix Hydration
This post is intended to complement the earlier Fibroblast post...essentially an attempt to provide some ¨digestible¨ amounts of critical information on the fundamentals of connective tissue (fascia). It can be somewhat overwhelaming, however it isn´t necessary to attempt to completely unravel the entire story...rather to acquire a working knowledge and understanding so that intelligent formulation, analysis, and strategy can be generated. The following information is quite readily available from many sources, but hopefully I will be able to compress it into an easily absorbable ¨blurb¨.
Connective Tissue (CT) composes a large amount of total body mass and contributes to a wide variety of important systemic and mechanical functions ranging from support, movement, fluid transport, and various metabolic processes. The unique properties of the CT are determined by the extracellular matrix (ECM). The ECM is essentially made up of 3 major macromolecules: Fibers (Collagen, Elastin), Proteoglycans, and Glycoproteins (not necessary to remember these). It is also made up of tissue fuid. The before mentioned Fibroblast exists within this matrix as well. All of these components are linked and contribute to the mechanical role (systemic as well) of connective tissue. Connective tissue responds (through Mechanotransduction) to compression, tension, sheer, and torsion...therefore the type of response in directly linked to the TYPE OF IMPOSED STIMULUS. The ECM therefore regulates the tissue environment based on the stress it experiences. One way this is done is by regulating fluid flow.
Fluid flow refreshes the tissue and promotes elasticity as well as healthy remodelling. Impairments to fluid flow are linked to extreme conditions such as fibrotic conditions (lack of effective fluid flow) and edema (intrusion of excess fluid). The fuid within CT is made up of free moving and bound water molecules, therefore its mobility is dependant on slower / lighter inputs of stimulus (stress).
The above image is an example of Trans-Fascial Viscolelastic Stimulation (TFVES) which is speciafically designed to promote healthy remodelling of connective tissue through the use of a stress transfer medium (Soft Gym Ball). The technique itself has specific loading properties that promote the transfer of mechanical stimulus to the deeper fascial levels. It is this movement of interstitial fluid that drives the remodelling process and contributes to the strengthening of the connective (fascial) system. It has been shown that collagen synthesis continues up to 48 hours after applied stimulus, which higlights the very specific nature of connective tissue response---more isn´t necessarily better.
It is important to remember that equilibrium between collagen synthesis and degradation is essential for proper function (systemic and mechanical). Any alteration in this homeostasis results in systemic dysfunction, metabolic deficiencies, irregular mechanical loading and force transfer --- essentially the entire spectrum of potential pathology from osteoarthritis, rheumatoid arthritis, and extending into disorders of movement and posture (Cerebral Palsy). In summary, each of the theoretical posts found here (Mechanotransduction, The Fibroblast, Connective Tissue) are meant to serve as pieces to the larger picture --- specific, focused stimulus applied in a specific way to achieve a specific desired goal. Each topic stands alone, however the fundamental thing to rememeber is to make links and draw strategic conclusions that make sense. More to come. Cheers.
The above image is an example of Trans-Fascial Viscolelastic Stimulation (TFVES) which is speciafically designed to promote healthy remodelling of connective tissue through the use of a stress transfer medium (Soft Gym Ball). The technique itself has specific loading properties that promote the transfer of mechanical stimulus to the deeper fascial levels. It is this movement of interstitial fluid that drives the remodelling process and contributes to the strengthening of the connective (fascial) system. It has been shown that collagen synthesis continues up to 48 hours after applied stimulus, which higlights the very specific nature of connective tissue response---more isn´t necessarily better.
It is important to remember that equilibrium between collagen synthesis and degradation is essential for proper function (systemic and mechanical). Any alteration in this homeostasis results in systemic dysfunction, metabolic deficiencies, irregular mechanical loading and force transfer --- essentially the entire spectrum of potential pathology from osteoarthritis, rheumatoid arthritis, and extending into disorders of movement and posture (Cerebral Palsy). In summary, each of the theoretical posts found here (Mechanotransduction, The Fibroblast, Connective Tissue) are meant to serve as pieces to the larger picture --- specific, focused stimulus applied in a specific way to achieve a specific desired goal. Each topic stands alone, however the fundamental thing to rememeber is to make links and draw strategic conclusions that make sense. More to come. Cheers.
Thursday, May 3, 2012
Everything you learned about fitness is wrong.
Thus begins my attempt to delve back into the realm of fitness...with a title that some will perceive as controversial, arrogant, or otherwise ¨entertaining¨. To be clear, this title is intended to catch attention...to convert potential disinterest into some level of curiosity. I have found that the fitness industry (in general) is a very ¨protective¨ entity...and therefore is sometimes slow to the idea of reformulating their ¨good old standards¨. What it does succeed in doing is bringing the otherwise bland, boring, and tasteless scientific concepts to the mainstream. It is cleverly packaged and marketed so that the masses find it irresistible...regardless of the actual scientific validity (or even whether it works or not).
I will therefore make another attempt to jump right into an industry that, in my opinion, has an opportunity to evolve exponentially. Given that it is largely unregulated, the simple idea of having some fundamental principles in place (as well as a philosophy that makes sense!) is only logical.
Before any expanded theory or concept, the most important starting point is to have intelligent SOURCES of information...therefore this small post will serve this purpose. Check out the Balance Fitness Facebook page http://www.facebook.com/pages/Balance-Fitness/162287483873151 as well as Fitnophrenia.blogspot.com.
In the coming weeks, I am hoping that interest grows and therefore I will begin my long rant as to why everything you learned is wrong. To be more accurate (and diplomatic): Everything you learned about fitness can be upgraded.
Cheers!
Subscribe to:
Comments (Atom)