Thursday, May 31, 2012
Effects of Load-Bearing in Cerebral Palsy: Bones
The intent of this post is two-fold: 1) to discuss and explore a very relevant, critical, yet controversial subject of dicussion within Cerebral Palsy (CP) (and other disorders of movement and posture)...2) to link previous posts together with this one to shape a formulate the overall narrative. As always, my overall intention is not to discredit any particular school of thought, strategy, or central philosophy...rather to bring the realities of the mechanical challenegs (and consequences) that accompany CP to the forefront so that specific, goal-oriented strategies can be formulated. It should be clear that these strategies are case specific and therefore need to be evaluated with it´s own set of standards.
This first installment will focus on the direct effect of load-bearing (weight-bearing) on the bones. However, before any in-depth discussion begins, I should define what load-bearing means within the context of this post. To be very specific, load bearing is: exposing an architectural system to structural load or stress. Therefore, in the human organism this is very clearly achived in either a seated or standing position.
The benefits of load bearing or weight bearing in the healthy person are quite obvious and straightforward...the ground force reaction promotes to development of growing bones and contributes to the development of healthy bone density. Although this is very true, the fundamental mistake that is quite often made is that this statement is imported to the CP community. Why is this a mistake? This statement assumes that the transmission of ground force reaction is efficient and therefore travels to the relevant load bearing structures throughout the body...in disorders of movement and posture (CP, for example), force transmission is extremely disrupted and inefficient. This disruption leads to improper stress distribution, accessory and compensatory activation of skeletal muscle, overuse and fatigue syndromes, as well as structural deterioration. To be very clear: mechanical forces in the CP individual DO NOT travel in a manner that facilitates healthy growth and development.
I doubt any responsible professional would debate this fact...however, a fundamental question is therefore raised: if this is an understandable fact, why is there such a rush to implement "standing" protocols? This is a glaring contradiction that generally goes unseen, but certainly exists...and therefore needs to be addressed.
In order to address this delicate topic intelligently and responsibly, we need to dissect the effects of load bearing into some fundamental component parts: the effect on the bony skeleton itself and the effect on the soft tissue. The effects on the system as a whole are actually greater than the sum of the component parts, but far more complex...therefore a basic understanding of the component parts should give some clarity on the potential "biomechanical tax" that is paid when weight bearing is aggressively promoted.
MECHANOTRANSDUCTION IN BONES: If the term Mechanotransduction is new to you, i would refer you to my previous post titled "Mechanotransduction: Response to Manual Therapy". However, to summarize the concept, it is the cellular response to mechanical forces or loads. The precise mechanism in which bones sense mechanical stimulii is still largely being researched, however the concept of cellular mechanotransduction in the bones is widely accepted as a likely mechanism. With respect to the skeleton, there is an integration of the understanding of the connective tissue memebrane of the bone (periosteum), cellular tensegrity, and the effects of mechanotransduction on the nucleus of the osteoblast. Effectively, mechanical stress and deformation that is load-induced activates a change in the genetic program of the bone (gene transcription). Mechanical information is relayed from the bone to the gene by a succession of long-term deformation and changes in conformation. If the stresses applied to the bone are not distributed properly, skeletal growth and absorption are disrupted...which leads to eventual bony deformation and therefore impaired function.
Although this is a common understanding in the field of cellular biochemistry, it doesnt seem to reach the professional "masses" to be applied responsibly in rehabilitative protocols. Given this knowledge, it becomes clear that consistent, intensive, and aggressive strategies geared towards standing protocols (standers, for example) is potentially costly when you consider the "biomechanical tax" to be paid in the long-term. Although bony misalignment is a reality in the CP individual, load bearing and exposing an altered structural "scaffold" to loads exacerbates the deterioration of structural integrity.
Although significant, this is only part of the overall perspective. The effects of load bearing with respect to the soft-tissue will be the subject of the second load-bearing post. Hopefully both or either will stimulate some analytical thought on the subject and consequenty result in more informed and effective strategies.
Cheers.
Wednesday, May 23, 2012
The Activ8 System
After a few trials, many format changes, and quite a bit of hesitation...I have finally decided to present my long-overdue fitness protocol for professionals. I had originally presented it a year ago as Soft Plyometrics, however I have refined it in an effort to make it as compact and useful as possible. More importantly, something that can be implemented very easily and very quickly. The Activ8 System is a tool designed to tap the body´s undiscovered performance potential. It includes very specific strategies and guidelines, however it is fundamentally a philosophy. The philosophy is based in the idea that performance potential (and even general health) is multi-rooted and multi-faceted...therefore it simply cannot be fully cultivated unless each root and each facet are stimulated. The beauty of the Activ8 System is that it doesn´t ignore or disregard ANY other fitness paradigm...in fact, it absorbs it. It can be implemented as a complete health, wellness, or fitness platform...or it can be inserted as a compliment to any and all fitness protocol. The adaptability of Activ8 is due to the fact that it´s primary objective is the development of the most primitive and fundamental structures involved in human deveopment and performance: Connective Tissue. Beyond the obvious strategic objectives of increased strength, power, endurance...the connective tissue / fascial system is responsible for important elemental and integral functions such as fluid transport, metabolic homeostasis, and the regulation of the injury repair mechanism.
The full protocol will be unveiled here over time, however I will be attempting to initiate some trial runs with a couple of enlightened professionals (check out Fitnophrenia blog at getcrazyfit.blogspot.com as well as my good friend Simon at Balance Fitness on Facebook) ahead of time to get the ball rolling. Until then, the fundamentals of the Activ8 System should be outlined. As you may have guessed, there are 8 central objectives:
Strengthen. Develop and increase overall strength by promoting one of the fundamental elements in force transfer and distribution---Fascia. Relax. Implement effective and efficient active relaxation strategies to reduce muscular stress and fatigue. Nourish. Actively promote and assist the flow of nutrients throughout the body to increase regeneration and repair. Repair. Implementation of strategies to combat overuse syndromes, chronic and acute injury, inflammation, and the buildup of metabolic by-product. Facilitate. Facilitate and improve the positive effects of complimentary protocols and interventions. Support. Actively develop the primitive support structures that are used, not only in performance situations, but in daily life as well. Maintain. The maintenance of general health and metabolic homeostasis. Develop. Develop the fundamental building blocks for long term health and fitness.
More to come!
Tuesday, May 22, 2012
Stretching and Cerebral Palsy: What you should know.
This is something I would most certainly define as a ¨hot button topic¨. Although most would consider it a relatively straightforward issue, the reality is that there are many schools of thought on this particular issue...all of which typically claim to have the ¨correct¨ perspective on the subject. It has been my experience that most take an all-or-nothing approach...black or white...do or don´t...stretching in Cerebral Palsy (CP) is good / stretching in CP is bad. I certainly have a specific position in the matter, however I think it is more productive to for people (both professional and health care seeker) to arrive to their own conclusions and convictions. This relatively trivial and non-sensical debate becomes completely irrelevant once the reality of the CP condition is analyzed in any decent way. I don´t think that there is any requirement to go into detail about the implied rationale for stretching...this is something that, to say the least, is well understood. However, a broad look into ¨what is stretching¨ will help to frame the overall message of this post.
Stretching is most commonly performed to achieve a specific end result: elongation of a particular muscle or group of muscles. This seems relatively intuitive and would make sense to any lay person. The part that is not so intuitive is that the muscles themselves are embedded within a connective tissue matrix...which is in turn blended with other differentiated connective tissue (tendon) that is continuous with the outer layer (periosteum) of the bone. From there, the periosteum continues and eventually blends once again and the kinematic chain continues.
Therefore it becomes quite clear that it is next to impossible to selectively isolate muscle tissue from the connective tissue matrix / system it exists with..in fact, they are inseperable and synonymous with each other. In other words, ¨stretching the muscle¨ effectively results in applying tensional force throughout the entire system (muscle, epimysium, perimysium, fascia, tendon, ligament, periosteum, etc...). In order to further decontruct the entire stretching concept, the terms muscle and connective tissue need to be further defined.
Muscle is defined as a tissue composed of bundles of elongated cells capable of contraction and relaxation to produce movement. Connective Tissue can be descried as a tissue developed from the embryonic mesoderm that consists of collagen or elastic fibres, fibroblasts, fatty cells, etc., within a jelly-like extracellular matrix. It supports organs, fills the spaces between them, and forms tendons and ligaments. Knowing these basic facts and definitions, their respective functional appearances within the normal muscle and the spastic muscle (CP) need to be defined. They should be the same, right? This couldnt be further from the truth. This is what the current (and most popular)approach assumes...that muscle is muscle and fascia is fascia. I have attached a very interesting and informative study that was performed to identify the similarities / differences between spastic and normal muscle tissue, spastic and normal extracellular matrix, as well as the differences between individual cells and collective bundles of cells for both. I recommend that you take the time to read it, but I will summarize its contents here in an effort to expediate my point (it´s effectively the abstract of the article): 1) The difference between bundles and single cells was much greater in normal muscle tissue (16 times stronger) than in spastic muscle (2 times stronger). 2) Actual muscle fiber strength is greater in spastic muscle than in normal muscle. However..... 3) Extracellular matrix strength / Connective Tissue strength is 43.5 times weaker!! Therefore, the ¨inconvenient truth¨ is exposed and a fundamental question is raised: if the spastic muscle itself is stronger than normal muscle, and the connective tissue attachments are 43 times WEAKER...what is really happening when you attempt to stretch that particular muscle(s)? In my professional opinion, it seems only logical that the likely result is further weakening and de-stabilization of an already weak connective tissue system...however, I am more than willing to set that staunch opinion aside if ever there was a way to guarantee this wouldn´t happen. The current reality is that, at best, there is no definite way to determine if the attempts to relax spastic muscles via stretching will not potentially be of some detriment. Indeed, there are some cases where some relief has been attributed to active stretching...however, these responses are transient and were most likely done in a very mild form.
The article goes into more important details (muscle fiber size and area is smaller in spastic muscle, for example), so I will leave those for the more curious to digest. In summary, I do not belong to the extreme end of the continuum in saying that ¨all stretching is bad¨ and that it absolutely shouldnt be done. My main message is that proper consideration be made to the actual mechanical and physiological benefits / consequences of ANY therapeutic intervention. If, through careful thought, consideration, and analysis, stretching is indicated...then it is obviously worthy of implementation. The harsh reality is that many forms of stretching are dispensed without any constructive analysis...which is fundamentally dangerous. To put a final point on this topic...forget about absolute ¨black and white¨solutions. There is a whole lot of grey to choose from! Cheers! Inferior Mechanical Properties of Spastic Muscles Due to Compromised Extra Cellular Matrix Material
Stretching is most commonly performed to achieve a specific end result: elongation of a particular muscle or group of muscles. This seems relatively intuitive and would make sense to any lay person. The part that is not so intuitive is that the muscles themselves are embedded within a connective tissue matrix...which is in turn blended with other differentiated connective tissue (tendon) that is continuous with the outer layer (periosteum) of the bone. From there, the periosteum continues and eventually blends once again and the kinematic chain continues.
Therefore it becomes quite clear that it is next to impossible to selectively isolate muscle tissue from the connective tissue matrix / system it exists with..in fact, they are inseperable and synonymous with each other. In other words, ¨stretching the muscle¨ effectively results in applying tensional force throughout the entire system (muscle, epimysium, perimysium, fascia, tendon, ligament, periosteum, etc...). In order to further decontruct the entire stretching concept, the terms muscle and connective tissue need to be further defined.
Muscle is defined as a tissue composed of bundles of elongated cells capable of contraction and relaxation to produce movement. Connective Tissue can be descried as a tissue developed from the embryonic mesoderm that consists of collagen or elastic fibres, fibroblasts, fatty cells, etc., within a jelly-like extracellular matrix. It supports organs, fills the spaces between them, and forms tendons and ligaments. Knowing these basic facts and definitions, their respective functional appearances within the normal muscle and the spastic muscle (CP) need to be defined. They should be the same, right? This couldnt be further from the truth. This is what the current (and most popular)approach assumes...that muscle is muscle and fascia is fascia. I have attached a very interesting and informative study that was performed to identify the similarities / differences between spastic and normal muscle tissue, spastic and normal extracellular matrix, as well as the differences between individual cells and collective bundles of cells for both. I recommend that you take the time to read it, but I will summarize its contents here in an effort to expediate my point (it´s effectively the abstract of the article): 1) The difference between bundles and single cells was much greater in normal muscle tissue (16 times stronger) than in spastic muscle (2 times stronger). 2) Actual muscle fiber strength is greater in spastic muscle than in normal muscle. However..... 3) Extracellular matrix strength / Connective Tissue strength is 43.5 times weaker!! Therefore, the ¨inconvenient truth¨ is exposed and a fundamental question is raised: if the spastic muscle itself is stronger than normal muscle, and the connective tissue attachments are 43 times WEAKER...what is really happening when you attempt to stretch that particular muscle(s)? In my professional opinion, it seems only logical that the likely result is further weakening and de-stabilization of an already weak connective tissue system...however, I am more than willing to set that staunch opinion aside if ever there was a way to guarantee this wouldn´t happen. The current reality is that, at best, there is no definite way to determine if the attempts to relax spastic muscles via stretching will not potentially be of some detriment. Indeed, there are some cases where some relief has been attributed to active stretching...however, these responses are transient and were most likely done in a very mild form.
The article goes into more important details (muscle fiber size and area is smaller in spastic muscle, for example), so I will leave those for the more curious to digest. In summary, I do not belong to the extreme end of the continuum in saying that ¨all stretching is bad¨ and that it absolutely shouldnt be done. My main message is that proper consideration be made to the actual mechanical and physiological benefits / consequences of ANY therapeutic intervention. If, through careful thought, consideration, and analysis, stretching is indicated...then it is obviously worthy of implementation. The harsh reality is that many forms of stretching are dispensed without any constructive analysis...which is fundamentally dangerous. To put a final point on this topic...forget about absolute ¨black and white¨solutions. There is a whole lot of grey to choose from! Cheers! Inferior Mechanical Properties of Spastic Muscles Due to Compromised Extra Cellular Matrix Material
Wednesday, May 16, 2012
Life, Tensegrity, and Thermodynamics
The title of this post is likely to deter most casual readers and appeal to the few ¨nerds¨ out there...so I expect a relatively low number of reads. However, I hope it inspires some analytical thought and stimulates some curiosity. At the very least...it´s interesting!
I have to give credit to Mr. Serge Gracovetsky who is a well known researcher (from my home town of Montreal, no less) who has been well ahead of the curve with respect to ¨how the body really works¨. His enormous body of work is something to behold and should be an essential component to any serious clinician´s resource library. His insights and concepts are the essense behind this post...I simply ¨dumb them down¨ for my own consumption.
Although the terms Tensegrity and Thermodynamics are quite straightforward, ¨LIFE¨ is a term that is obviously something subject to interpretation...and therefore it is unlikely that a true ¨definition¨ will ever be found. However, in the functional sense, life is the convertion of heat into energy. Living organisms are essentially converters that transform heat into mechanical work. This convertion (heat into mechanical work) is extremely inefficient however...the classic steam engine was only 3% efficient!! This is due to the Second Law of Thermodynamics: Energy continuosly degrades and is less and less available for work. This energy loss is called ENTROPY. Since energy is continuosly lost, entropy increases over time.
In order for life to exist (and persist), this energy loss and entropy has to be minimized...therefore ¨life¨ exists in the most energy efficient and low energy cost state (for example, water, salts and minerals crystallize) that is also stable. Therefore...as Gracovetsky states...To survive the animal must minimize its energy needs, that is minimize the rate at which the entropy increases.
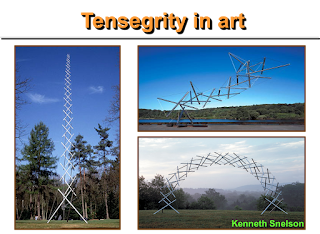
What does this all mean? Organisms driven purely by muscle would be efficient in a fluid medium (like fish, for example...essentially all muscle and very little solid bone and connective tissue), however in a gravitational field (on the earth) muscles are extremely expensive energy users. Therefore, LIFE has blessed us with Tensegrity...which essentially allows us to be upright in a gravitational field without using muscles all the time. Tensegrity is a technique for building structures by decomposing forces into their compressive and tensile components.
The marvel of tensegral structures is that they are highly adaptable to stress and can therefore support loads without experiencing structural failure. Within the human organism, one of the most prevalent tensile structures is Collagen.
In summary, this simple realization should signal a radical shift in current ¨standards¨ of practice in traditional rehabilitative sciences. It essentially presents a challenge to the conventional, classicla representation and modelling of biomechanical systems (Gracovetsky).
Mr. Gracovetsky could not have summarized this very important point more clearly: The response of tissues under stress should not be limited to the mechanical properties of the tissues, but should include the dynamic reconfiguration of the collagen network. Such a desirable analysis is unfortunately not the norm in the literature.
...Hopefully a good read for nerds and non-nerds alike!
Cheers!
Tuesday, May 8, 2012
Connective Tissue: Extracellular Matrix Hydration
This post is intended to complement the earlier Fibroblast post...essentially an attempt to provide some ¨digestible¨ amounts of critical information on the fundamentals of connective tissue (fascia). It can be somewhat overwhelaming, however it isn´t necessary to attempt to completely unravel the entire story...rather to acquire a working knowledge and understanding so that intelligent formulation, analysis, and strategy can be generated. The following information is quite readily available from many sources, but hopefully I will be able to compress it into an easily absorbable ¨blurb¨.
Connective Tissue (CT) composes a large amount of total body mass and contributes to a wide variety of important systemic and mechanical functions ranging from support, movement, fluid transport, and various metabolic processes. The unique properties of the CT are determined by the extracellular matrix (ECM). The ECM is essentially made up of 3 major macromolecules: Fibers (Collagen, Elastin), Proteoglycans, and Glycoproteins (not necessary to remember these). It is also made up of tissue fuid. The before mentioned Fibroblast exists within this matrix as well. All of these components are linked and contribute to the mechanical role (systemic as well) of connective tissue. Connective tissue responds (through Mechanotransduction) to compression, tension, sheer, and torsion...therefore the type of response in directly linked to the TYPE OF IMPOSED STIMULUS. The ECM therefore regulates the tissue environment based on the stress it experiences. One way this is done is by regulating fluid flow.
Fluid flow refreshes the tissue and promotes elasticity as well as healthy remodelling. Impairments to fluid flow are linked to extreme conditions such as fibrotic conditions (lack of effective fluid flow) and edema (intrusion of excess fluid). The fuid within CT is made up of free moving and bound water molecules, therefore its mobility is dependant on slower / lighter inputs of stimulus (stress).
The above image is an example of Trans-Fascial Viscolelastic Stimulation (TFVES) which is speciafically designed to promote healthy remodelling of connective tissue through the use of a stress transfer medium (Soft Gym Ball). The technique itself has specific loading properties that promote the transfer of mechanical stimulus to the deeper fascial levels. It is this movement of interstitial fluid that drives the remodelling process and contributes to the strengthening of the connective (fascial) system. It has been shown that collagen synthesis continues up to 48 hours after applied stimulus, which higlights the very specific nature of connective tissue response---more isn´t necessarily better.
It is important to remember that equilibrium between collagen synthesis and degradation is essential for proper function (systemic and mechanical). Any alteration in this homeostasis results in systemic dysfunction, metabolic deficiencies, irregular mechanical loading and force transfer --- essentially the entire spectrum of potential pathology from osteoarthritis, rheumatoid arthritis, and extending into disorders of movement and posture (Cerebral Palsy). In summary, each of the theoretical posts found here (Mechanotransduction, The Fibroblast, Connective Tissue) are meant to serve as pieces to the larger picture --- specific, focused stimulus applied in a specific way to achieve a specific desired goal. Each topic stands alone, however the fundamental thing to rememeber is to make links and draw strategic conclusions that make sense. More to come. Cheers.
The above image is an example of Trans-Fascial Viscolelastic Stimulation (TFVES) which is speciafically designed to promote healthy remodelling of connective tissue through the use of a stress transfer medium (Soft Gym Ball). The technique itself has specific loading properties that promote the transfer of mechanical stimulus to the deeper fascial levels. It is this movement of interstitial fluid that drives the remodelling process and contributes to the strengthening of the connective (fascial) system. It has been shown that collagen synthesis continues up to 48 hours after applied stimulus, which higlights the very specific nature of connective tissue response---more isn´t necessarily better.
It is important to remember that equilibrium between collagen synthesis and degradation is essential for proper function (systemic and mechanical). Any alteration in this homeostasis results in systemic dysfunction, metabolic deficiencies, irregular mechanical loading and force transfer --- essentially the entire spectrum of potential pathology from osteoarthritis, rheumatoid arthritis, and extending into disorders of movement and posture (Cerebral Palsy). In summary, each of the theoretical posts found here (Mechanotransduction, The Fibroblast, Connective Tissue) are meant to serve as pieces to the larger picture --- specific, focused stimulus applied in a specific way to achieve a specific desired goal. Each topic stands alone, however the fundamental thing to rememeber is to make links and draw strategic conclusions that make sense. More to come. Cheers.
Thursday, May 3, 2012
Everything you learned about fitness is wrong.
Thus begins my attempt to delve back into the realm of fitness...with a title that some will perceive as controversial, arrogant, or otherwise ¨entertaining¨. To be clear, this title is intended to catch attention...to convert potential disinterest into some level of curiosity. I have found that the fitness industry (in general) is a very ¨protective¨ entity...and therefore is sometimes slow to the idea of reformulating their ¨good old standards¨. What it does succeed in doing is bringing the otherwise bland, boring, and tasteless scientific concepts to the mainstream. It is cleverly packaged and marketed so that the masses find it irresistible...regardless of the actual scientific validity (or even whether it works or not).
I will therefore make another attempt to jump right into an industry that, in my opinion, has an opportunity to evolve exponentially. Given that it is largely unregulated, the simple idea of having some fundamental principles in place (as well as a philosophy that makes sense!) is only logical.
Before any expanded theory or concept, the most important starting point is to have intelligent SOURCES of information...therefore this small post will serve this purpose. Check out the Balance Fitness Facebook page http://www.facebook.com/pages/Balance-Fitness/162287483873151 as well as Fitnophrenia.blogspot.com.
In the coming weeks, I am hoping that interest grows and therefore I will begin my long rant as to why everything you learned is wrong. To be more accurate (and diplomatic): Everything you learned about fitness can be upgraded.
Cheers!
Sunday, April 29, 2012
The "New" Understanding of Anatomy: Pre-Stressed Systems
PRE-STRESSED SYSTEMS: The first installment of the ¨Wheel¨ series is an introduction to a fundamental characteristic of complex biological systems. The very definition of ¨complex¨ indicates that these types of systems are difficult to de-construction and effectively understand...therefore I will present this specific characteristic in a more straight-forward and ¨simplistic¨ way.
It is important to realize and understand the fundamental difference between organic and inorganic structures. This statement may seem trivial...of course there is a difference...however, the reality (and experience) shows that this logic goes completely out the window when we examine conventional rehabilitative strategies. Simple mathematical models and equations can successfully be applied to simple (inorganic) structures without any significant concern for error. The inconvenient reality is that these same simple mathematical models (lever classes, axis of rotation, range of motion, etc) are being ¨imported¨ to represent complex organic systems...as if they were both the same. This is effectively where the proverbial ¨boat¨ gets missed. Effective rehabilitation strategies hinge on understanding the fundamentals of the organic ¨Superstructure¨...which is a structure that is PRE-STRESSED.
Pre-stressed systems are characterized by a built-in tensional component that allows it to respond / adjust to the changing environment and, consequently, the internal forces it generates. This phenomenon is ironically all around us...and can be observed every single day. For example, the earthquake that struck Haiti a couple of years ago left the entire country devastated. It was a large magnitude quake that left the buildings in ruins and rubble. However, a significantly larger quake hit Chile...and even with the larger, taller buildings almost none of them came down. Why? The buildings are built PRE-STRESSED. Therefore, ground force reaction (represented by the earthquake) is efficiently distributed throughout the entire system and permits the building to adjust. How is this applicable to the human body and rehabilitation? Let´s move into some specifics:
A simple wagon wheel is a rigidly made structure that is essentially built for obvious purposes. This is a good example of a non-stressed structure.
When it rolls along the ground, the individual spoke (and the rim in contact with the ground) take absorb the ground force reaction while the other spokes do nothing. In effect, the entire weight of the wheel (and therefore all of the ground-force reaction) goes through a relatively small area. This illustrates the ¨Support comes from the bottom¨ mantra...as the bottom part of the wheel provides 100% of the support for the movement.
A bicycle wheel, although functionally equivalent to the wagon wheel, is a much more sophisticated and efficient contruction. The spokes of a bicycle wheel are PRE-STRESSED...therefore they have a pre-existing tensional component to them (green arrows).
As the wheel rolls, ground force reaction enters from the bottom, thereby reducing the tension on the bottom spokes...which consequently results in an INCREASE IN TENSIONAL SUPPORT FROM THE UPPER SPOKES. This global response allows the wheel to absorb significantly more force and stress without failing (breaking). The question may arise again: How in the world is this applicable? The body is not a bicycle wheel! Indeed, it is not...but it IS pre-stressed!
As ground-forces are imposed into the system from the bottom, the reaction is the same. The tensional support (tensegral) comes from the top. This is easily observed by placing your fingers between the trochanter and iliac bone and walking a few steps. As you heel strike, you will feel a palpable increase in tension. This is a counter-intuitive reaction and can therefore create some relative confusion. However, a study of pre-stressed systems (as well as a delve into Biotensegrity) will reveal that this is by far the most accurate representation of how complex systems work. Therefore, a radical shift in rehabilitative assessment and evaluation is in order. Traditional ¨proven¨ techniques such as gait analysis do not take this into account...therefore produce very diluted and simplistic strategies. If we take this realization further and quickly examine the sitting position, the Tensegral / Pre-stressed paradigm takes on a much more tangible role.
When seated, support will be derived from the top. As the ground forces are imposed on the pelvis, the entire system will adjust accordingly. In summary, the entire framework of ¨rehabilitation¨ needs to be established based on how the body actually works. The current health care delivery system is geared to address the masses...and therefore needs to be simplified to the most common denominator and provide strategies that fit the majority. However as INDIVIDUAL helath care providers, we need to make a concerned effort to customize our protocols towards strategies based in fundamentals of the human organism. I hope I have been somewhat successful in delivering this important message. Part 2 will continue the exploration into compex systems and attempt to draw links and bridge gaps. Cheers!
A simple wagon wheel is a rigidly made structure that is essentially built for obvious purposes. This is a good example of a non-stressed structure.
When it rolls along the ground, the individual spoke (and the rim in contact with the ground) take absorb the ground force reaction while the other spokes do nothing. In effect, the entire weight of the wheel (and therefore all of the ground-force reaction) goes through a relatively small area. This illustrates the ¨Support comes from the bottom¨ mantra...as the bottom part of the wheel provides 100% of the support for the movement.
A bicycle wheel, although functionally equivalent to the wagon wheel, is a much more sophisticated and efficient contruction. The spokes of a bicycle wheel are PRE-STRESSED...therefore they have a pre-existing tensional component to them (green arrows).
As the wheel rolls, ground force reaction enters from the bottom, thereby reducing the tension on the bottom spokes...which consequently results in an INCREASE IN TENSIONAL SUPPORT FROM THE UPPER SPOKES. This global response allows the wheel to absorb significantly more force and stress without failing (breaking). The question may arise again: How in the world is this applicable? The body is not a bicycle wheel! Indeed, it is not...but it IS pre-stressed!
As ground-forces are imposed into the system from the bottom, the reaction is the same. The tensional support (tensegral) comes from the top. This is easily observed by placing your fingers between the trochanter and iliac bone and walking a few steps. As you heel strike, you will feel a palpable increase in tension. This is a counter-intuitive reaction and can therefore create some relative confusion. However, a study of pre-stressed systems (as well as a delve into Biotensegrity) will reveal that this is by far the most accurate representation of how complex systems work. Therefore, a radical shift in rehabilitative assessment and evaluation is in order. Traditional ¨proven¨ techniques such as gait analysis do not take this into account...therefore produce very diluted and simplistic strategies. If we take this realization further and quickly examine the sitting position, the Tensegral / Pre-stressed paradigm takes on a much more tangible role.
When seated, support will be derived from the top. As the ground forces are imposed on the pelvis, the entire system will adjust accordingly. In summary, the entire framework of ¨rehabilitation¨ needs to be established based on how the body actually works. The current health care delivery system is geared to address the masses...and therefore needs to be simplified to the most common denominator and provide strategies that fit the majority. However as INDIVIDUAL helath care providers, we need to make a concerned effort to customize our protocols towards strategies based in fundamentals of the human organism. I hope I have been somewhat successful in delivering this important message. Part 2 will continue the exploration into compex systems and attempt to draw links and bridge gaps. Cheers!
Monday, April 16, 2012
Gravity is the Therapist
I have been quite busy recently and have neglected my blogging duties, however the last 2 weeks have produced quite a bit of enlightened moments and "ah-hah" revelations. I have found that information is more effectively delivered in "digestible chunks", therefore I have decided to ease into the next topic with a brief blurb on the overall topic: GROUND FORCE REACTION AND LOAD BEARING. This is a rather long title only because I havent been able to formulate anything that encompasses my line of thought yet...but I'm sure it will materialize very soon!
I read a quote some time ago that I found, not only to be quite clever, but surprisingly accurate: Gravity is the therapist. The quote was followed by a more expanded description of the underlying message. Essentially, ground force reactions are the derivative of gravitational force...which contributes in a positive way to our functional development. However, if the structure through which these reaction forces travel are weak or misalignment, gravity becomes our worst enemy. This promotes further destabilization of the joints, increases muscular imbalances, results in the physiological stress-shielding effect, and ultimately perpetuates the degenerative cycle.
The upcoming posts will take a deeper look into the actual reality of load bearing and ground-force reactions. In addition, they will introduce an analytical approach that will leave some intrigued, scratching their heads, or otherwise confused...but hopefully there will be some "AH HAH" moments generated as well!
I consider this a brief introduction to the upcoming series I have titled as "Re-inventing The Wheel"...which will be delivered in separate parts to avoid "reading indigestion". I hope you tune in and read!
PS: For those ABR family readers...this series will definitely be relevant.
Cheers!
Saturday, March 24, 2012
Re-Defining the Joint: Part 3
It has been quite awhile since the posting of part 1 and part 2, however there has been a recent ¨spike¨ in reads for both parts (currently rank #2 and #9 in the top 10 reads) therefore I think it is an appropriate time to complete the trilogy. As per part 1 and 2, a radical alteration of conceptual understanding of joints must take place in order to fully grasp (and appreciate) the complexity of human movement.
I read a book called The Structure of Scientific Revolutions that effectively demonstrates a ¨fatal¨ flaw in the evolution of science...most (if not all) of the new ¨scientific discoveries¨ are derived from already established paradigms. To be specific, research into human movement and (bio)mechanics assumes that the traditional mathematical model (single pivotal movement) is the ¨law¨...therefore every hypothesis, design, conclusion is derived from this ¨fact¨. Common sense dictates that, if the overriding paradigm is flawed (or otherwise over-simplified), then the results / conclusions will also be so. Although over-simplification has some merit in making treatment protocols easier to ¨digest¨and conform to current health care delivery methods, it does not mean than more precise and effective understanding should be ignored. In fact, deeper understanding does not disregard the current formula...rather it ABSORBS IT.
In order to fully appreciate part 3, I suggest a read (or re-read) of parts 1 and 2. However, to summarize the main message:
The true definition of a joint must be expanded into a broader understanding that it is the linear or angular displacement between separate biological elements. Therefore, simple pivotal movement is only a fraction of the equation. There are 2 fundamental realities that also exist alongside of the classical mathematical model:
1) Fascial Articulations: This term defines the very real movement potential between the individual fascial layers that exist from the surface of the skin to the periosteum of the bone (and indeed even deeper into the very cell itself).
The above image illustrates an example of the fascial relationship between muscle/tendon and adjacent structures. Effective movement requires, not only proper ¨connective¨ elements, but selective ¨DISCONNECTIVE¨ properties. In other words, the ¨sliding¨ (hence articulation) of fascial layers between each other is essential. By definition, this constitutes a joint...without these characteristics, movement potential is significantly altered leading to movement dysfunction, irregualr load bearing and stress distribution, and ultimately deterioration.
2) Movement is more precisely ¨Gear-like¨: This is perhaps confusing and counter-intuitive, however it is none-the-less a reality. The pivotal model suggests that movement is a summation of single pivots moving at the same time. Once again, this is a serious over-simplification.
True function is achieved through a complex of gear-like movements that are NOT the sum of individual movements rather a single unified systemic response.
The image to the left clearly illustrates that single pivotal movement (hip joint) is effectively a small contributor to the performance of a straight leg raise (hip flexion). This movement is defined by gear-like movement between the individual vertebrae of the lumbar spine, the pelvis, and the hip. In addition, this requires proper fascial articulation (sliding) of the fascial layers of the posterior leg.
It is precisely these realities that highlight some of the current flaws in assessment and evaluation protocols. The fundamental question remmains: how can an effective treatment protocol be formulated when only one third of the mechanism is observed and identified??! At best, these types of approaches will be successful only 33% of the time and/or resolve only 33% of the initial problem. The concept of re-defining the definition of a joint only serves to enhance understanding and by default result in more effective interventions.
The switch from pivotal understanding to the ¨gear ratio¨ perspective will provide some valuable insight and clarity into the amazing movement potential of the human body. I am reminded of an ¨Old School¨ kids game called Spirograph. My brother and I played with this quite alot, but it has its merits from a conceptual perspective.
It involved placing variuos small gear-like tools into the center of a larger circle with gear teeth. You would then insert pencils of different colour into the smaller gear and spin it around the outer circle. The result was a myriad of amazing shapes and images.
Although it is a simplistic analogy, it reveals the sophistication and complexity that exists in this model...whch is reflected in the everyday marvel of human movement.
I hope this trilogy has been both informative and insightful. If nothing else, it serves as an example of the need to reach beyond current accepted paradigms in an effort to evolve your understanding.
Cheers.
Saturday, March 17, 2012
The Student Becomes The Teacher
Every once in awhile it is good to stop and engage in some serious introspection. I mean this from a purely professional perspective. To be precise, the designation of ¨professional¨ assumes some level of competency that is superior to that of those who seek your help. On some levels this is true...however, the harsh reality is that many take this too seriously. I truly believe that true professionalism is the CONTINUING search for more understanding as well as being conscious of the fact that there is so much more yet to learn.
It is in this light from which the inspiration for this short post was formulated. I am once again working with the ever-enthusiastic ABR (Advanced Biomechanical Rehabilitation) families from Rosario, Argentina and I experienced a very encouraging event. My role with these families is, at it´s essence, that of a coach or mentor...however this time I was pleasantly surprised to be the student for a short time! For those who are unfamiliar with ABR, it is a very innovative technique that is taught to the parents of children with Cerebral Palsy (and other disorders of movement and posture) so that they are able to deliver consistent and comprehensive treatment directly in the home. There are a multitude of applications and guidelines that require regular skill development for which I am responsible for providing.
Each individual child is unique in their priorities, manifestations, and challenges...which makes the implementation of each application unique in itself. On some occasions, particular applications can be challenging and can sometimes present some difficulties to us ¨coaches¨. I was therefore very encouraged when I saw a father (Ivan Cief...a naturally skilled ABR provider) performing his own version of a particular application. This inspiration came from intelligent and analytical thinking on how to best deliver a specific technique (Submerged Shoulder) given the unique characteristics of his daughter.
It is then that I put on my ¨student´s hat¨ and grabbed my camera. Ivan´s carefully formulated adjustment opened the door to some very interesting and new possibilities for positioning that will hopefully be translated into future improvements and evolution of the technique. I will be (unofficially) calling this the ¨Uma Position¨...which will be a continuing reminder that some cliche´s (however much we hate to hear them) are true: the best teachers learn from their students!
Hats off to Ivan and Team Uma!
Monday, February 27, 2012
The Fibroblast
Another brief rant on the fundamentals of understanding the role of fascia and connective tissue. Although there are many specific topics to uncover, there isnt a better place to start than getting familiar with the Fibroblast.
A fibroblast is a cell that essentially produces and maintains the Extracellular Matrix of the connective tissue...or to put it simply, the ¨caretakers¨ of the connective tissue. It does this by secreting precursors into the extracellular matrix which maintain the structural integrity of the entire system.
The most important characteristic to remember about the Fibroblast is that it is adaptive. They provide the architectural plan for the fascial system and therefore react and adapt to tensional / compressional (Tensegral) stress. Through Mechanotransduction (see previous post: Mechanotransduction), it can transmit forces within the cell as well as from cell to cell through tensional forces. Why is this so important? Fibroblasts provide the architectural framework for bones, nerves, blood, fascia, etc...and therefore all of the structures that depend on those structures.
It is important to remember that the specific adaptation exhibited by the fibroblast is dependant on the mechanical force applied...therefore rendering the type of intervention (also the mode of intervention) a critical consideration for the care-seeker.
In most disorders of movement and posture (Cerebral Palsy, etc) and even most chronic pain disorders, there is a significant weakness / dysfunction of the connective tissue system. This is manifest a a pure weakness of the tissue itself or in a symptomatic way (muscular tension as a result of connective tissue fatigue or failure).
In summary, understanding the fundamental ¨building blocks¨ provides valuable insight into the development, management, and maintenance of the megstructure.
Cheers!
Tuesday, February 14, 2012
The ¨SuperTendon¨ Concept
Once again, I have been bitten by the ¨nerd bug¨and have been plowing through some of the scientific articles that are continually piling up...with no end in sight. I consider this both a blessing and a curse: although it is obvious that I do not possess enough years in my lifetime to absorb everything, each new read sheds even more light and understanding.
I have recently been examining the ¨Form and Function¨relationship...more specifically, the concept that form (structure) IS function. With this in mind, I came to focus on a particular article that had previously gone unnoticed. Upon reading through it, I was pleasantly surprised to finally find a ¨user-friendly¨ article that captures the essence of the Transanatomical understanding of human form and function. To be precise, it exposes the limits of the popular Topographical Anatomy understanding when it comes to analyzing function...which therefore renders any rehabilitative strategy to something relatively simplistic.
It is through works like this...as well as the mentioned Frederic Wood Jones and Buckminster Fuller...that we get a more comprehensive understanding of the intimate relationship between the ¨Bioengineering¨of the human organism (form) and our interaction with the environment (function). More to come on the works of Wood Jones and Fuller, but this article should provide an effective entry into the transanatomical mindset.
Structure-Function Relationships in Tendons
Thursday, February 9, 2012
Success in the Fascial Paradigm: Passive-Aggressive Therapy?
I have chosen this photo to lead off this post for a very straightforward reason: it is time for the "therapeutic world" to take off the noise-cancelling headphones and start to acknowledge the undeniable potential of the fascial paradigm in the treatment of Cerebral Palsy and other disorders of movement and posture.
I think it is EXTREMELY important to also acknowledge the generous and unselfish contribution of Nancy and Haroldo Guerrero who have given me permission to use the images of their child to further contribute to the overall good and education of families and professionals alike. It has been my honour and pleasure to have been able to work with them for the last 4 years...and I am humbled by their dedication, work ethic, and superior frame of mind. Therefore on behalf of myself and all of the readers of this post...GRACIAS, NANCY Y HAROLDO!
Although a comprehensive history is always recommended, I will abbreviate this particular history in an effort to remain within a "digestible" amount of information. Matias is a severely affected child who obviously manifests a great deal of musculoskeletal challenges. This manifestation is most easily observed as muscular tension, rigidity, and stiffness. Within the traditional musculoskeletal paradigm, this tension is considered the "problem" therefore it is given primary focus and is the target of selective intervention (stretching, Botox, surgery, tenotomy, etc). As mentioned before in this blog (see previous post "Spastic Muscles: Victim or Perpetrator"), the muscles are SYMPTOMATIC. Therefore, they REFLECT an underlying problem and are therefore considered victims. By definiton, it is unproductive to set them as the primary rehabilitative focus. The true "perpetrator" is the lack of compressional strength (postural strength) which is mediated by the fascial system. There will be a large number of people / professionals scratching their head at this statement..."that doesn't make any sense whatsoever". With all due respect to them, my simple reply would be that it doesnt make sense to them because that's not what they read in their textbooks! My best advice would be to close those books...look at things more analytically...and formulate your own conclusions. This in itself is a difficult task...therefore I propose a simpler approach which comes in the form of a simple fundamental question that you should ask yourself: IS IT POSSIBLE TO IMPROVE THE STRUCTURE OF A SEVERELY AFFECTED CP CHILD WITHOUT ATTACKING THE MUSCLES THEMSELVES? As you should have already guessed...my answer is a resounding YES!
This simple fact leaves no denying that a more passive, less invasive / aggressive should always be considered first. I admit that simple words are rarely enough, so I am very happy to share some very positive results on what can be generally considered a difficult case.
For those who are not familiar with the Scribd program I use for posting documents: You must click the title (in blue) of the document to download it. You will likely be able to read it directly from my blog, just use the scroll bar on the right hand side. It may be small lettering for some...so please be sure to click and have a look directly on Scribd if necessary!
Success in the Fascial Paradigm
Thursday, February 2, 2012
Mechanotransduction: Response to Manual Therapy
For the very few regular readers, I must apologize for the long delay between posts. My unofficial rule is to produce 3 or 4 posts per month...however it seems that newborn babies do not follow this rule! Now that I have had a few months to adjust, recharge, and refocus, I will begin my "re-entry" into the blogosphere with a short back to basics post.
I have recently been clicking through the Inger Lab web publications (a very good site for those fascia nerds like me) and I came to the realization that a great deal of information is right under our noses...it just requires some effort in "digging" for it. What do I mean by this? Most people have the obvious and instinctive understanding that "if I go to get manual therapy, I will feel better". For most, this basic understanding is sufficient...for example, I need not know HOW a touchpad on a computer works. I need only know that that it does indeed work. But for the more investigative mind (both care-giver and care-seeker), the question still remains "how does the active manipulation of tissue translate into an immediate (or long-term) response? The answer is MECHANOTRANSDUCTION. To put it simply, Mechanotransduction is the process by which cells (and therefore tissue itself) sense mechanical stress and convert these stresses into biochemical signals. On a cellular level, the signal is sent to the nucleus and thus affecting the tissue on a "macro" level by promoting healthy remodelling.
As the above image so elegantly illustrates, the cell itself is a Tensegral construction that intimately connects the entire organism. Depending on the type of stress (sheer, compression, tension, etc), the cell will respond differently. Therefore, the TYPE of manual application is vitally important as well as the MODE of delivery (light, aggressive, quick, slow, etc).
With respect to the Fascial Paradigm, this is a key understanding and fundamental principle. Remodelling of connective tissue is always the ultimate goal, however the promotion of HEALTHY remodelling is the key.
My parting message is simple: Even the smallest biological element (cell) can sense differences in mechanical stress. Therefore the focus on the characteristics of the application of the manual therapy technique become more than important...they are critical! Mechanotransduction shows us that there is true power in the effectiveness of manual therapy...the real "skill" comes with the understanding of the specific mechanisms of application and response.
Thanks for reading!
Sunday, November 20, 2011
Cerebral Palsy and the Pediatric Evaluation
Part 2: The Developmental Process: Primitive and Postural Reactions
The second installment in this series on Understanding the Pediatric Evaluation revolves around two fundamental elements of the developmental process that are critical in the greater understanding of the long-term rehabilitation plan. Primitive and postural reactions are characteristic of critical early development that effectively signal progression and movement towards improved development. They are the easiest, earliest, and more frequently used tools in assessing neurological and motor development in newborns and infants.
Primitve Reactions
Primitive reactions are mediated in the brainstem and are fully present at birth. They are characterized by automatic movement patterns that become more difficult to elicit after the first 4-6 months of life. Some examples below:
Moro Reaction: The Moro reaction is obtained by holding the baby’s head and shoulders off of the mat with the arms held in flexion on the chest. The examiner suddenly lets the head and shoulders drop back a few inches while releasing the arms. The arms should fully abduct and extend, then return towards the midline with the hand open and the thumb and the index finger forming a “C” shape. An absent or incomplete Moro is seen in upper motor neuron lesions.
Prone: In the prone position, the baby should be able to extend the neck to the point where the head can be turned side to side. When the arms are extended by the side of the trunk, the baby should be able to bring them forward into a flexed position. The buttock should be somewhat elevated because the hips are flexed and adducted. A baby that is flat on the mat and can’t turn the head back and forth has low tone and weakness.
Head Lag: Starting in the supine position, the baby is pulled by the arms to the sitting position. The head and the arms are observed during the maneuver. The arms should remain partially flexed at the elbow and the head may lag behind the trunk, but should not be fully flexed backwards. When the baby is in the sitting position, the head should be able to come to the upright position for at least a few seconds before dropping forward or backward.
Postural Reactions
Postural Reactions develop following / during the disappearance of the primitive reactions. They can be considered voluntary actions that are produced by multiple sensory and structural inputs. They are complex motor responses to afferents like tendons, joints, skin, internal organs, and even the eyes and ears. They are characterized by predictable postural adjustments to specific applied sudden changes in position. As the child develops, the postural reactions (or postural performance) improve and manifest in more comprehensive ways as he /she ages. Some examples below:
Head and Trunk Control: When pulled to a sitting position, a baby this age should be able to have only slight head lag and, when sitting, the head should be upright but there may still be some wobbling of the head. The back is still rounded, so the baby slumps forward.
Prone: In the prone position, the baby is now able to bring his head up and look forward with the head being 45 to 90 degrees off the mat. Weight is borne on the forearms. When the head and chest are well off the mat, the baby is ready to start to roll from the prone to the supine position. Rolling front to back usually occurs at 3 to 5 months of age. Rolling over too early can be due to excessive extensor tone.
Lateral Propping: Lateral propping or protective extension is essential for the baby to be able to sit independently. This postural reaction develops at 5 to 7 months of age. Anterior propping actually develops first, then lateral propping. For anterior propping the baby will extend the arms forward to catch himself and prevent falling forward. Lateral propping occurs when the baby is falling to one side or the other and he extends the arm laterally to catch himself.
The understanding of these reactions is fundamental in the effective and accurate assessment of the success of the rehabilitation protocol. To be more precise, Infants with cerebral palsy have been known to manifest persistence or delay in the disappearance of primitive reflexes and pathologic or absent postural reactions. Therefore, the emergence of postural reactions (and the reduction of primitive reactions) is the primary treatment goal and thus any protocol that promotes this will ultimately contribute to improved function.
Part 1 of this series identified the need to place primary focus on the developmental age rather than the chronological age. Although not age appropriate, the persistent appearance of primitive reactions in older children is simply an indication of their current status and placement along the developmental path. It should also be remembered that the actual "manifestation" of these primitive reactions may look significantly different in an older child than a 6 month old. The structural proportions (length, weight, mechanics, torque, etc) are very different, therefore the same "reaction" may subjectively appear to be more severe or, at times, appear to be something completely different.
What does this all mean and how does it apply to my understanding of Cerebral Palsy? The answer is quite simple and straight-forward: the developmental process is something that cannot be circumvented or skipped. If the child with Cerebral Palsy continues to manifest primitive reactions in conjunction with the absence of postural reactions,any expectations of higher order function (crawling, independant sitting, gross / fine motor skills) is unrealistic. Rather than a message of "gloomy reality", the fundamentals of the development of the human organism will allow you to understand the "right path" and therefore effectively reduce any unecessary anxiety and worry associated with the unknown. More importantly, it clearly identifies those interventions that are essentially "shortcuts" along the path...which initially produce increased levels of hope and expectation, but in the end reduce maximum potential.
I apologize for the relatively longer post...it has been quite the challenge to even keep it this short! The third installement: Cerebral Palsy and the Pediatric Evaluation: A Case Study Report will blend the theoretical elements of part 1 and 2 and demonstrate their application in a practical examination of the progress of an actual CP child. I hope that it achieves my goal of creating a link and close the loop of understanding.
Saturday, November 12, 2011
Success story in progress
I am pleased to share a post from one of my ABR families who just recently finished a training session a couple of weeks ago here in Rosario, Argentina. Over the last couple of years, I have had the pleasure and honour to participate in Salvi's evaluations...and at each step he demonstrates continued progress and improvement. I recommend that everyone have a look at this post...but further to that, take time to browse the blog itself. The insight into a family's challenges and successes will be invaluable to anyone. Click the blue link below and enjoy. Cheers!
Creciendo con Salvi: Evaluación ABR noviembre 2011: Es muy difícil para mí intentar resumir todo lo que se habló en la última evaluación de Salvador. Fue muy intensa para mí, con muchísimo fun...
Saturday, November 5, 2011
Cerebral Palsy: Understanding the Pediatric Evaluation
Part 1: Fundamentals in Perspective
I thought it would be a good idea to begin this series of posts with a certain aspect that, in my opinion, is typically missing from most people when entering into any form of evaluation or assessment. It is not my intention to pass judgement on parents, professionals, or any other group of people...it simply exists. What is the missing ingredient? Perspective. Quite simply, the expectations of every parent with a child with CP must be tempered by the proper perspective. Without it, expectations can often run wild and ultimately lead to dashed hopes and unecessary feelings of guilt, frustration, and desperation.
Therefore, the question becomes: "What is the proper perspective?". The answer has been right in front of our (parents and professionals alike) noses. Conditions such as Cerebral Palsy, West Syndrome, etc...fall under the umbrella of Developmental Delay. Simply put, there is a significant delay in the development of healthy motor function. This is a reality that is inescapable...as chronological age proceeds at a regular pace, the developmental process lags behind. Therefore, by definition, the progression of each developmental phase is the ONLY component that matters when gauging progress. It is essential to remember that EVERYONE must pass through these developmental stages...irrespective of their chronological age. The very definition speaks for itself: Developmental Delay (CP) is characterized by the persistence or delay in the disappearance of
primitive reactions and pathologic or absent postural reactions. The vast majority of parents are focused in on the chronological age of their child and therefore attribute "age appropriate" expectations for their child. As mentioned in one of my previous posts: focused attention to your child's developmental age will give you the proper perspective on how they are "hardwired" to develop and therefore foster realistic expectations going into each evaluation or assessment.
Hopefully this small introduction serves to facilitate efficient absorption of the elements in Part 2 (The Developmental Process: Primitive and Postural Reactions).
Cheers!
Saturday, October 22, 2011
Pediatric Evaluation 101
I typically avoid back-to-back posts...prefering to let a post "marinate" in the minds of the reader for at least a week. However, I have recently been actively involved with my work with children with Cerebral Palsy (ABR) and it has only recently occured to me that alot of our evaluation protocol is still somewhat foreign to the many parents and family members. The purpose has become so integrated in my mind, that I haven't truly considered that anyone wouldn't understand, not only WHAT I'm doing, but WHY I'm doing it. In essense, I have overlooked an essential element of any successful assessment: UNDERSTANDING BY THE PARENT / CARE-SEEKER.
With this in mind, I have decided to post a series of "back to school" postings designed specifically to EDUCATE parents on the essentials of typical pediatric assessment protocols. It is my firm belief that, with understanding, you will become more involved in the process of your child's development. In this spirit, I have used a photo of Concordia University in Montreal at the beginning of this post. Not only did I receive my Bachelor of Science degree there, but I went on to teach as a laboratory instructor for 5 fun-filled years. So....class, attention please:
The first "class" is simply to familiarize you with a few basic tests and give you some insight into its purpose. Before I continue, I will remind you of an important point I raised in a posting from June (Trainers Corner: Back to Basics): Consider your child's developmental age in light of the chronological age. In children with disorders of movement and posture, improvement is gauged by the progressive movement through developmental milestones. Therefore, the normal developmental process is your guide. The following are some select tests, with their respective rationale and corresponding developmental stages:
The Prone Position: In the prone position, the baby is now able to bring his head up and look forward with the head being 45 to 90 degrees off the mat. Weight is borne on the forearms. When the head and chest are well off the mat, the baby is ready to start to roll from the prone to the supine position. Rolling front to back usually occurs at 3 to 5 months of age. Rolling over too early can be due to excessive extensor tone. In essense, any functional performance that includes rolling or propping on the hands is dependant on this prior stage.
The Landau Reflex: The Landau is an important postural reflex and should develop by 4 to 5 months of age. When the infant is suspended by the examiner’s hand in the prone position, the head will extend above the plane of the trunk. The trunk is straight and the legs are extended so the baby is opposing gravity. When the examiner pushes the head into flexion, the legs drop into flexion. When the head is released, the head and legs will return to the extended position. The development of postural reflexes is essential for independent sitting and walking. This particular test is not typically done, but can be valuable when more comprehensive discussion on sitting and walking become realistic.
Lateral Propping: Lateral propping or protective extension is essential for the baby to be able to sit independently. This postural reflex develops at 5 to 7 months of age. Anterior propping actually develops first, then lateral propping. For anterior propping the baby will extend the arms forward to catch himself and prevent falling forward. Lateral propping occurs when the baby is falling to one side or the other and he extends the arm laterally to catch himself. Asymmetric lateral propping can be an early sign of hemiparesis. The baby will prop on one side but on the paretic side he will not extend the arm to catch himself.
The Parachute Test (Flying Test): The parachute reflex is the last of the postural reflexes to develop. It usually appears at 8 to 9 months of age. When the baby is turned face down towards the mat, the arms will extend as if the baby is trying to catch himself. Prior to developing this reflex, the baby will actually bring the arms back to the plane of the body and away from the mat.
Traction Test: On traction, which is pulling to a sitting position, the baby has good head and trunk control. The head and shoulders are flexed forward and the arms are flexed. The baby actively helps himself to get to the sitting position by pulling with the arms. Also notice that the legs are flexed at the hips and are off the mat as the baby pulls himself to sitting. On being laid back down to the supine position, the baby doesn’t flop back, but is able to control the lowering of his head and trunk to the mat. This particular test should be very familiar to the ABR readers. How is "good head control" assessed? More importantly, what are the bare essentials needed to have minimal head control? The traction test is a valuable tool that gives excellent feedback and lends towards a more efficient treatment protocol.
In North America, coffee is just as important to the learning process as is a laptop...so, grab a cup of "Joe" (for my South American friends, un cafe con leche) and get to work.
Class dismissed.
Cheers! =)
Subscribe to:
Posts (Atom)